Life Sciences

From Chapter 10: A Tale of Six Cities
We used to think that the only risk factors for cardiovascular disease were genetics and diet. Few suspected that the air we breathe might be a risk factor too. It’s a simple matter of perception. The food we eat and beverages we drink are tangible, while the air we breathe is not, even though on any given day the air we inhale weighs up to ten times the amount of food and liquid we ingest. Let’s see... Twelve to twenty-five inhalations per minute, each having a volume of 1 liter (about 1 quart), gives approximately 20,000 liters of air taken into the lungs each day. One cubic meter of air weighs 1.2 kilograms (2.6 pounds), so 20 kilograms (44 pounds) of air pass daily through an adult’s body, in contrast to 1 kilogram (2.2 pounds) of solid food and 2 liters (2 quarts) of liquid.
Furthermore, infants breathe, eat, and drink up to three times as much as adults in proportion to their body weight. Young children, therefore, are exposed to much higher concentrations of pollutants than are adults.
It took until the 1970s to prove that smoking is toxic and until the 2000s to learn that exposure to secondhand smoke increases the risk of vascular diseases by 25 percent. This discovery spurred research on the association between urban air pollution, secondhand smoke, and heart disease. But proving that air pollution causes atherosclerosis, heart attacks, and strokes was no easy task; researchers encountered numerous obstacles.
Except in cases of extreme smog that can turn the center of a city into a gas chamber overnight, the effects of chronic exposure to air pollution may take decades to become manifest. Researchers had to observe whole cities for years in order to draw conclusions.
Exposure rates vary geographically and are difficult to measure. Tobacco exposure is much easier to quantify: researchers only have to count the number of cigarettes smoked in order to calculate the exposure, the risk, and the connection between the two.
Finding funding for research on the association between air pollution and cvd is difficult because the traditional sources for medical research, primarily the pharmaceutical industry, have little financial incentive to invest. Pharmaceutical and other industrial products cannot cure air pollution. The financial burden has therefore fallen on public sources and private sponsors concerned with the environment. Fortunately, many such agencies and patrons have stepped up to the platefor example the Guzzo family of Montreal, founders of the Guzzo cinema chain and sponsors of the Guzzo EnvironmentCancer Research Chair at the University of Montreal.
Finally, to demonstrate the toxicity of fossil-fuel burning is to challenge prevailing notions of industrial progress and invoke resistance from influential corporate interests. We know how powerful this resistance can be because we have seen it at work in the tobacco, soft-drink, and asbestos industries.
Despite all of these obstacles, researchers persisted, and the evidence began to pile up. When in June 2010 the American Heart Association released a major update on the association between air pollution and heart disease, no fewer than 426 scientific studies had been reviewed by leading experts in cardio-environmental health.1 Here briefly is a review of the findings of some of the most compelling of these studies.
Perhaps the pioneering study on the causes of cvd was the Harvard Six Cities Study (hscs), published in 1993 in the New England Journal of Medicine.2 The full story of this remarkable study may be found on the website of the Harvard School of Public Health,3 but let me mention the highlights. Several tenacious Harvard researchers launched their ambitious project in 1973. For sixteen years they followed 8,111 adults in six American cities (Watertown, Massachusetts; Harriman, Tennessee; St. Louis, Missouri; Steubenville, Ohio; Portage, Wisconsin; and Topeka, Kansas), collecting data on a variety of indicators: age, weight, sex, lifestyle (including smoking), and social and medical history. The researchers measured exposure levels to fine airborne particulate matter, acid aerosols, sulfur dioxide, and nitrogen dioxide. They tracked the mortality statistics. This study was like Framingham but from an environmental perspective.
The authors found that the cardiovascular mortality rate in the survey city with the most pollution was 25 percent higher than the rate in the city with the least pollution, all other factors being equal. The premature deaths from air-pollution exposure were linked to lung cancer in 8 percent of cases and to cardiovascular disease in 55 percent of casesthe first time this link was reported. It is useful to note that the 25 percent difference in mortality was recorded between two American cities in which inhabitants had similar lifestyles. It would be interesting to set up a comparison in which one of the cities had very little or no pollution. The data from such a study would be especially pertinent for cardiology.
Since the Harvard Six Cities Study was first published in 1993, hundreds of corroborating studies have come out, and we now know a great deal about the precise mechanisms and role played by air pollution in cardiovascular health.
***
Stress: a Heart Stopper
Stress is indeed bad for the heart, but the real culprit is oxidative stress, not the stress that most people think of when they hear the word (a somewhat minor and controversial risk factor, often confused with depression, a known risk factor). Air pollution contributes to the oxidation in the arteries in the same way that oxidation leads to rust in a metal pipe. In arteries, oxidative stress results in inflammation and atherosclerotic plaquearterial rustthe fatty substance that interventional cardiologists squeeze aside with stents.
How, physically, does this oxidation occur? When we breathe air containing pollutants released during fossil-fuel combustion, we take in a mixture of gases and very small particles called particulate matter (pm). Airborne particulate matter is categorized according to size: large particulates have a diameter of 10 microns (pm10) or less, fine particulates are 2.5 microns (pm2.5) or less, and ultrafine particulates are 0.1 microns (pm0.1) or less.
Human arteries are vulnerable to attack by atmospheric hazards precisely because ultrafine particulates are small enough to be carried deep into the lungs and, from there, to make their way into the bloodstream. (The membranes of the lung are finer and more permeable than those of the digestive tract.) Here these fine particulates come into contact with the arterial endothelium, the inner membrane of the arteries, whose role it is to protect and regulate the arterial system. If the endothelium reacts to the particles with inflammation, both short-term and long-term damage may result.
Also entering the body by the same pathwayand causing oxidative stressare toxic, unstable molecules known as free radicals. In the bloodstream they are usually triggered by such gaseous pollutants as ozone, sulfur dioxide, nitrogen dioxide, and carbon monoxide. Other airborne contaminants that may affect our health include volatile organic compounds (vocs) and polycyclic aromatic hydrocarbons (pahs).
In the lungs and arteries, all of these compounds can induce oxidative stress and inflammation, a condition similar to the chemical pneumonitis that afflicts firefighters who inhale smoke from burning buildings. In response, the body produces inflammatory proteinsinterleukin, cytokines, C-reactive proteinwhich in turn damage the inner and mid-level lining of the arteries.
Plant Technology of First Peoples of British Columbia

Plants of British Columbia
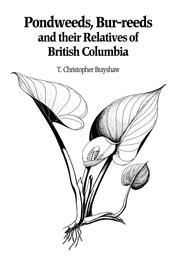
Pondweeds, Bur-reeds and Their Relatives of British Columbia